Background:
– Know the context for examining cranial nerves
– How much can they cooperate for examination?
– Use age-appropriate props, toys or distraction
– Developmental disorder?
– Acute / Chronic neurological symptoms?
– Syndromic child?
– Severely unwell child?
– What key information is needed from Cranial N exam?
1st N (Olfactory N)
– Enquire loss of smell
– Test for anosmia
2nd Cranial N (Optic N) tests:
– Visual acuity
Snellens/ finger counting
Near vision (small fonts)
– Colour vision (Ischiara charts)
– Light reflexes (Pupils)
Direct/ indirect/ accomodation
– Visual fields- any defects?
– Fundoscopy (optic N appearance)
Eye movements ‘H shaped’ (3rd, 4th & 6th N)
Unilateral 3rd N palsy (Occulomotor N):
– Ptosis
– Dilated pupil
– Eye deviated down & out
Unilateral 4th N palsy (Trochlear N):
Superior Oblique Palsy
– Diplopia
– Head tilt to compensate
Unilateral 6th N palsy (Abducens N):
Lateral Rectus palsy
– Diplopia on gazing in
– Eye unable to abduct
Facial sensations= 5th N (Trigeminal N)
– Sensations in 3 areas: Ophthalmic (& cornea), Maxillary, Mandibular
– Motor tests for Masseter muscle & test Jaw jerk
Facial movements= 7th N (Facial N)
– Raise eyebrows
UMN innervates both sides of forehead
– Shut eyelids forcefully
– Grin/ smile/ show teeth
– Puff/ blow cheeks
– Unilat tear/ saliva control?
also test sensation in ant 2/3 tongue
8th N (Vestibulocochlear)
– Enquire balance issues
– Rinne/ Weber
hearing tests
Palate/ Pharynx movements
9th N (Glossopharyngeal N)
– Absent Gag reflex?
– Unsafe swallow
10th N (Vagal N)
– Uvula raise (say Ahh..)
deviates to Normalside
11th N (Spinal accessory)
– Shrug shoulders
– Turn head to each side against resistance
Tongue movements= 12th N (Hypoglossal N)
– Observe fasciculations
– Move tongue side to side. Tip of tongue deviates to affected side
– Know the context for examining neurology
– Acute / Chronic neurological symptoms?
– How much can they cooperate for examination?
– Use age-appropriate props, or toys
– Record GCS/APVU, mini mental status
– Known developmental disorder/ Syndrome
– Unusual skin marks- cafe au lait, etc?
– Spine exam- scoliosis?
– Signs of meningitis?
– Measure & plot head circumference
Inspection
– Observe resting posture
– Observe spontaneous movements
smooth, coordinated movements?
Any splints, walking aids visible?
– Muscle mass
Any asymmetry?
Wasting of small muscles?
Hypertrophy (esp calves)
– Any fasciculations
– Involuntary movement?
Spasms, tremors, tics?
Sensation:
Know the dermatomes to test*
– Light touch
– Pain
– Temperature
– Vibration
– Proprioception
Cortical sensations:
– Steriognosis
– Tactile discrimination
Tone:
Resting posture- ‘frog like’
Baby handles like ‘rag doll’?
Head lag on ‘pull-to-sit’?
Ventral suspension- raises head?
Slipping if held under arms?
Abnormal ‘primitive’ reflexes?
Check ‘full range’ of joint movement
Passive tone with fast movements
– Normal / low tone?
– Any spasticity / cog-wheel rigidity?
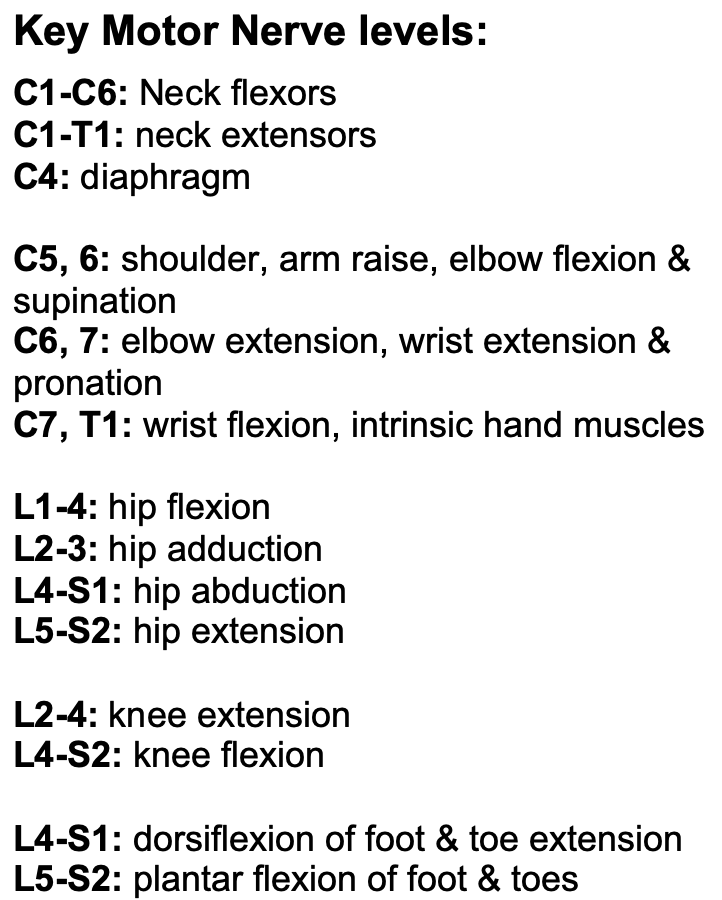
Power:
UL- Shoulders, Elbows, Wrists, fingers, thumb
LL- Hips, Knees, Ankles
Know joint movements & muscle groups
Classify power as:
0= No movement
1= Flicker only
2= Horizontal movement
3= Anti-gravity movement
4= Against some resistance
5= Against full resistance
Deep Tendon Reflexes:
Know technique to elicit DTR
Child comfortable with semi-flexed joint
– Biceps C5
– Brachioradialis C5, C6
– Triceps C7
– Knee L4
– Ankle S1
Babinski/ Plantar upgoing?
Complete examination with Gait & Coordination tests
Background:
– Acute ataxia or dysarthria?
– New focal neurological deficit?
– Chronic neurological symptoms?
– Can they cooperate for examination?
– Use age-appropriate props, or toys
– Record GCS/APVU, mini mental status
– Developmental disorder/ Syndrome
– Signs of meningitis?
– Measure & plot head circumference
Inspection
– Observe resting posture
– Observe spontaneous movements
smooth, coordinated movements?
Any splints, walking aids visible?
– Involuntary movement?
Spasms, tremors, tics?
– Any new weakness?
Standing balance (Romberg’s)
– Unsteady with eyes open= Cerebellar
– Unsteady after eyes closed= Sensory ataxia
GAIT: observe walking bare-feet
– Speed & symmetry of walking
– Swing and Stance phases
– Heel contact on floor (or flat foot or forefoot contact)
– Stability of posture/ swaying?
– Able to turn around?
– Walk on tip-toes & heels?
– Tandem walking along straight line with small steps
Gait abnormalities:
– Foot drop (peripheral neuropathy)
– Stiff, circumduction (spasticity)
– Wide unsteady (sensory apraxia)
– Slow initiation, shuffling (parkinsonism)
– Waddling/ pelvic sagging (myopathy)
– Abnormal tandem walk (Cerebellar)
Cerebellar tests:
Upper limb (hand eye coordination)
Observe past-pointing & intention tremors
– Handwriting sample available?
– Colouring / drawing shapes
– Able to eat snacks
– Finger nose test
– Dysdiadochokinesia (rapid alternate hand tapping)
Lower limbs
– Heel to shin test
– Standing balance/ Gait tests (as above)