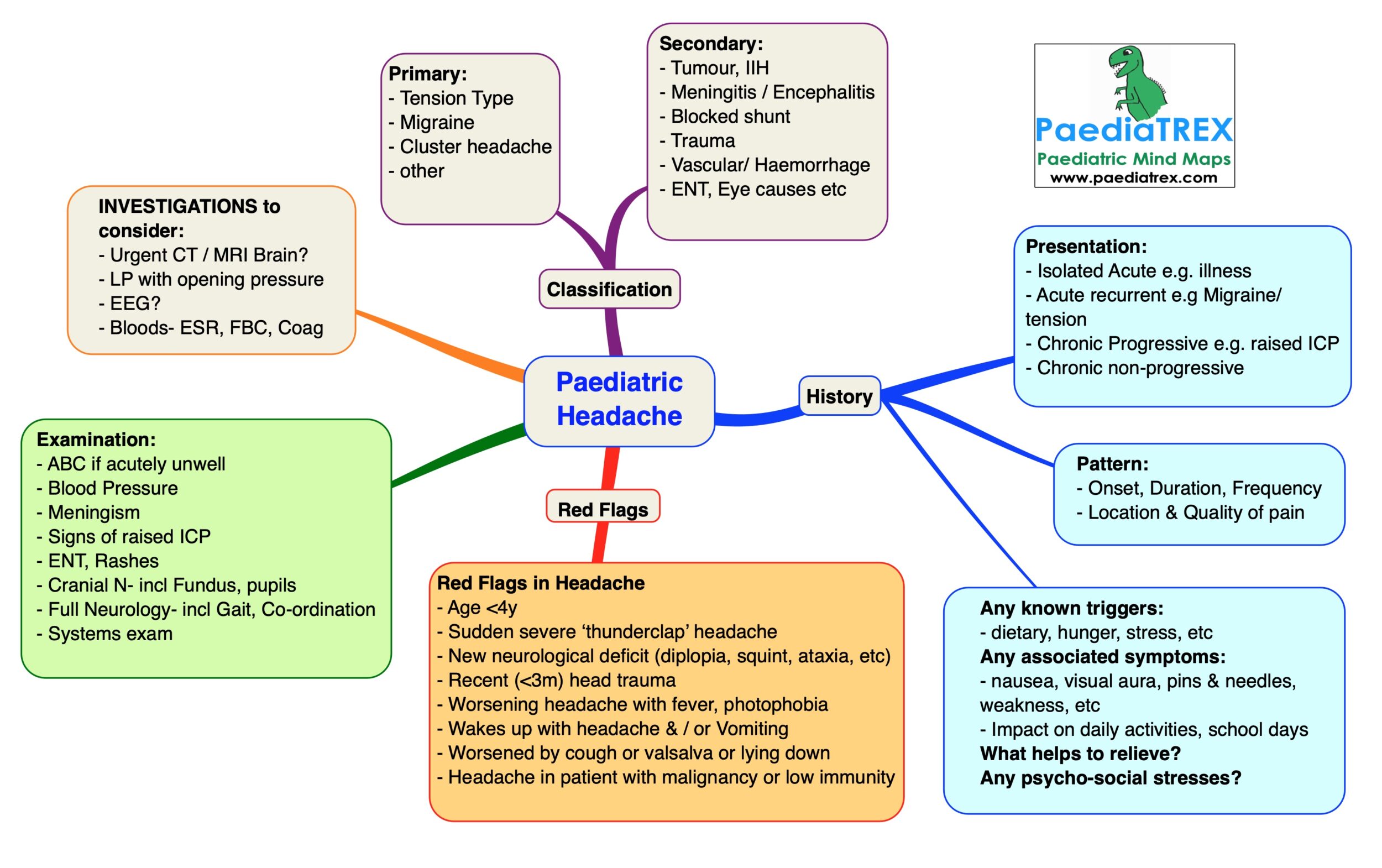
Headache in childhood
Primary:
– Tension Type
– Migraine
– Cluster headache
– other
Secondary:
– Tumour, IIH
– Meningitis / Encephalitis
– Blocked shunt
– Trauma
– Vascular/ Haemorrhage
– ENT, Eye causes etc
History:
– Onset (weeks or months)
– Duration of each episode (minutes, hours or days)
– Frequency of episodes (daily or infrequent)
– Location & type of pain
Pattern over time:
– Isolated acute headache e.g. illness
– Acute recurrent e.g Migraine/ tension
– Chronic Progressive e.g. raised ICP
– Chronic non-progressive
Any known triggers: dietary, hunger, stress, etc
Any associated symptoms: nausea, visual aura, pins & needles, weakness, etc
What helps to relieve headache?
Any psychosocial stress factors (at home or school)? Impact on daily activities, school days
Examination:
– ABC if acutely unwell
– Blood Pressure
– Meningism
– Signs of raised ICP
– ENT, Rashes
– Cranial N- incl Fundus, pupils
– Full Neurology- incl Gait, Co-ordination
– Systems exam
Red Flags in Headache:
– Age <4y
– Sudden severe ‘thunderclap’ headache
– New neurological deficit (diplopia, squint, ataxia, etc)
– Recent (<3m) head trauma
– Worsening headache with fever, photophobia
– Wakeing up with headache or Vomiting
– Worsened by cough or valsalva or lying down
– Headache in patient with malignancy or low immunity
Investigations to consider:
– Urgent CT / MRI Brain
– LP with opening pressure
– EEG?
– Bloods- ESR, FBC, Coagulation profile
