Lymphadenopathy in a child
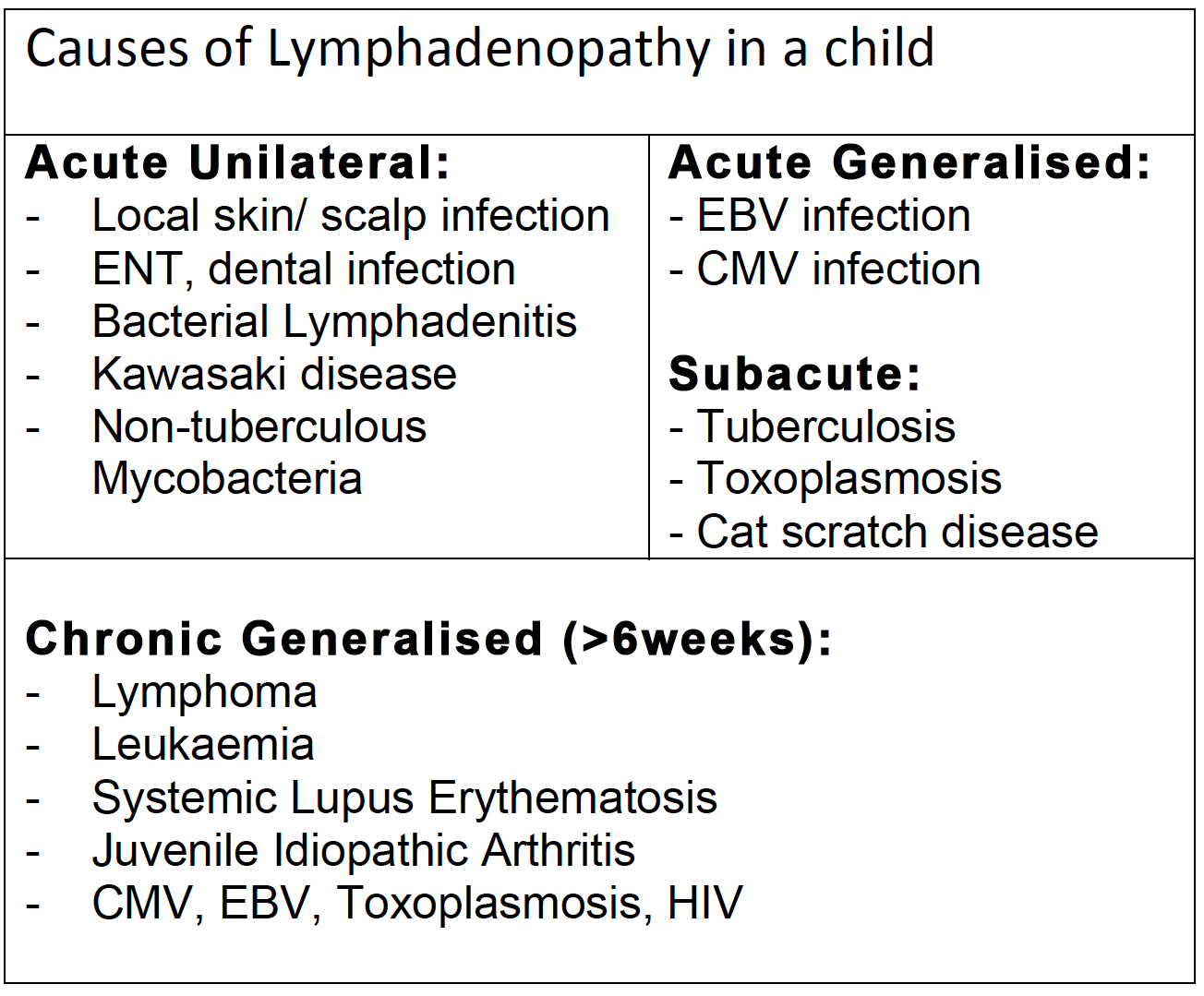
Referral for cervical lymphadenopathy is a common one and is generally related to localised infections.
History:
– LN how many lumps? painful? redness?
– Fever, rigors?, rash?
– Sore throat, cough, dental pain?
– Eczema, Skin infection?
– Is HIV/ STD possible?
– Any weight loss, night sweats?
– Pallor, bruising, bone pain?
– Fatigue, itchiness, joint pains
– Headaches, vomiting, blurred vision?
– Exposure to TB or farm animals?
– Recent travel
– Any known underlying illness
Examination:
– Looking ill, pale, miserable, unwell?
– LN description– size, site/s
unilateral/ bilat/ generalised
tender? erythematous?
fluctuant? firm/ rubbery/ matted?
– ENT exam
– Eczema, rashes, bruises?
– Respiratory distress?
– Abdo mass?, Hepato-spleenomegaly
Red Flags:
– LN continuing to grow > 2 weeks
– Persistently > 2cm after 4 – 6 weeks
– Not reduced to <1cm after 8 – 12 weeks
– Persistent fever >2 weeks
– Weight loss, fatigue, night sweats
– Bruising, bone pain, pallor
– Hepato-spleenomegaly
– Supraclavicular LN
Management:
Acute localised, arising from local infection:
– Empirical antibiotics, review in 48h
– Monitor for 2 – 4 weeks
– Consider Kawasaki if other features
Acute LN in unwell child:
– Consider FBC, film, U&E, CRP
– LFT if suspecting viral cause
– Blood cultures if systemically unwell
– Empirical antibiotics, review in 48h
– Consider further investigations
Consider biopsy if
>2cm, solid, matted
abnormal appearance on USS
suspected non-mycobacterium
suspected neoplasia
Chronic cervical LN at 6 weeks:
A) Well child & all nodes <1cm & mobile
= Reassure & discharge
B) If any of red flags:
– FBC, film, U&E, LFT
– Uric acid, LDH
– Serology for EBV, CMV, Toxoplas
– CXR, USS of LN, USS Abdo/Pelvis
– Consider referral to Oncology / ENT
