Fever in children
Feverish illnesses are a common paediatric presentation, and usually suggests infective cause especially in young children.
Babies and infants present a challenge in distinguishing simple causes from a serious bacterial infection or sepsis.
A thorough assessment is done to find and treat the focus of infection.
Most children have a minor childhood illness with a viral infection, but differentials include: Viral illness, LRTI, UTI, Gastroenteritis, Sepsis, meningitis, encephalitis, osteomyelitis, endocarditis etc
Remember rarer causes such as: Kawasaki disease, Rheumatic fever, JRA, TB, Malaria, etc
A fever without apparent cause that has persisted for >21 days is defined as ‘prolonged fever of unknown cause’. Consider non-infective causes such as Rheumatic fever, SLE, Malignancy, IBD, JRA, HIV etc
High risk groups include:
– Babies under 3m age with temp > 380C
– Children 3 – 6 m age with temp > 390C
– Children with Neutropenia or other immunocompromised state
– Children with complex chronic illnesses, including neurodisability
History
Elaborate fever duration pattern, presence of rigors, use of antipyretic and response
Ask parent’s concerns and perception of a fever in their child.
Enquire if feeding or drinking adequate fluids; passing adequate urine
Systemic features- cough-cold, earache, vomiting, diarrhea, any rashes, limping, joint swelling etc
Enquire ‘worrying’ symptoms of lethargy, irritability, breathlessness, poor colour, dehydration, etc
Any exposure to infections, ill contacts, travel abroad? Ask immunization history.
Examination
Any child with fever have triage / initial assessment to identify any immediately life threatening features with the standard ABCDE approach, including recording of Temp, HR, RR, CRT and SaO2 (Also BP if high HR or lethargy)
– Colour and hydration status
– ENT: any bulging TM or fluid collection behind TM or discharging ear; coryza; Tonsillar hypertrophy or pus spots
– Lymph nodes: localized?, Small or enlarged?, Fluctuant?, Is there generalized lymphadenopathy?
– Rash: blanching?, Localized or generalized?, Maculopapular or Vesicular?
– Anterior fontanelle: is it open?, Bulging or sunken?
– Spontaneous movement of all 4 limbs?, walking normally or limping?
– RS: Any crackles or wheeze?, Is there increased work of breathing?
– CVS: Any new murmur?
– PA: Any organomegaly?, Any other mass? See hernia sites
– CNS: Are pupils equal & reactive?, Any neck stiffness or meningism?, Any focal neurological abnormality? Seizures?
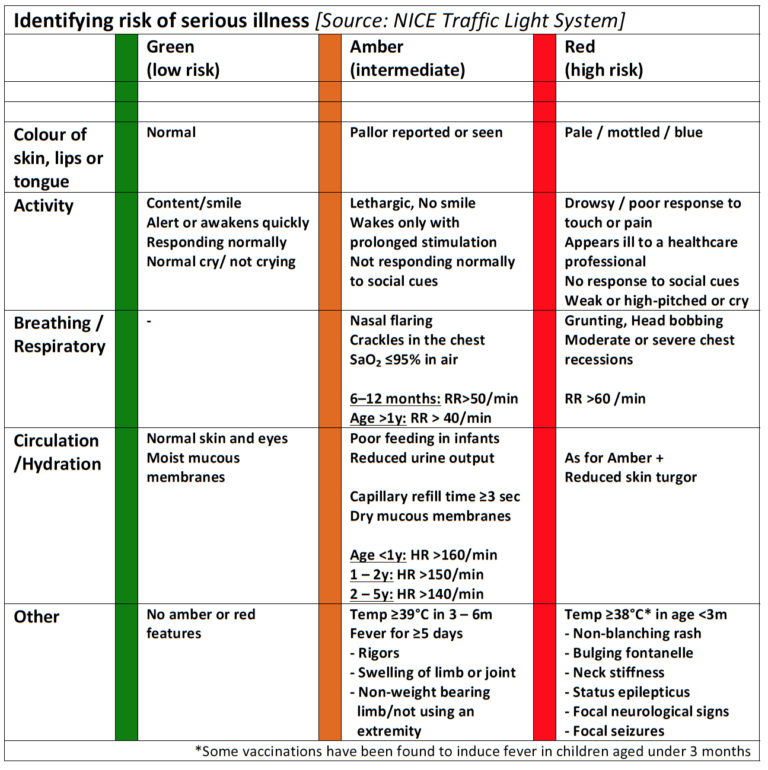
The NICE guidelines provide a helpful approach is triaging an unwell febrile child.
Investigations
The NICE traffic light tool is less useful in guiding investigations, so clinical judgement and senior advice is needed.
Investigations are guided by clinical assessment, age of child, specific circumstances and likelihood of sepsis.
Have a low threshold to investigate young children, those who appear unwell or those without a clear focus for cause of fever.
– FBC, U&E, CRP, Blood culture
– Consider Blood Gas, Lactate, Blood Glucose if child appears unwell
– Consider Urine culture in all young children (esp <3y age)
– Consider Lumbar puncture in young children (<3months as per NICE) if no contraindication. LP in older children if suspecting meningitis / encephalitis
– Consider Chest x-ray if respiratory signs present
– Consider stool culture if diarrhoea present
Other tests to consider case-by-case: LFT, Monospot/ EBV serology, Nasal secretions for virology or pertussis, ESR, Blood film thick smear for malaria parasites, USS abdomen and pelvis to look for collection, ECHO to exclude endocarditis.
Management
Admit / observer in short stay unit if:
– Any worrying features on assessment
– High parental anxiety or concern; social or family situation
– Staff concerns ‘gut instinct’ about serious illness
– Recent travel abroad, especially to a tropical country
– Child who is immunocompromised or has complex chronic illness
– No clear focus for fever
Observation for few hours is often helpful if there is diagnostic uncertainty, as repeating full examination once child is apyrexial may be needed.
Unwell / young children often are admitted with suspected sepsis, undergo septic screen and receive empirical antibiotics such as Cefotaxime or Ceftriaxone.
Consider Cefotaxime + Amoxycillin in neonates (to cover for Listeria)
Do not delay broad-spectrum antibiotics in children with suspected sepsis or meningitis.
Consider giving IV Aciclovir if suspecting herpes simplex encephalitis
Consider giving IV corticosteroid (>3months age) if bacterial meningitis confirmed on LP
Fever is managed with Paracetamol or Ibuprofen (not together) in those with high grade fever, those who appear unwell, lethargic or distressed with the temperature.
It is not necessary to reduce temperature in a well child. This should be discussed and agreed with parents.
Remember that antipyretic agents do not prevent febrile convulsions
Response to antipyretics does not always distinguish a serious illness from viral illness.
Discharging a child with fever:
Children who appear well on assessment, with clear cause for fever and no worrying (amber or red) features can be discharged home. Always provide advice on warning symptoms and signs to look out for- if possible written card.
Advice on feeding and temperature control.
Also advice when to return for further medical assessment, including contact details of department.
NICE Guideline. Fever in under 5s – assessment and initial management; (2017)
Thompson M, et al. Systematic review and validation of prediction rules for identifying children Health Technol Assess. 2012 Mar16(15):1-100
