Henoch – Schönlein Purpura
Henoch Schönlein Purpura (HSP) is the commonest childhood systemic small vessel vasculitis, most commonly young children (3-10 years). HSP is usually a self-limiting condition; and often occurs following an upper respiratory tract infection. Prognosis is only affected if renal involvement is present.
Differential Diagnoses:
– Sepsis (meningococcal)
– Thrombocytopenia
– Leukaemia
– other vasculitides (e.g. Wegener’s, SLE).
HSP presentation
Skin (100% involvement) – palpable purpuric rash.
– Often starts as macular-papular erythematous rash before evolving to petechiae and purple, non‐blanching, non‐pruritic urticarial, palpable purpuric lesions.
– Distributed symmetrically, mainly to extensor surfaces of legs and buttocks. Can also be present on arms, face and ears but usually spares the trunk
– Rarely subcutaneous oedemaof the scalp, ears, periorbital area, dorsi of the hands and feet and genitalia (young children) and haemorrhagic bullae.
GI tract
– Abdominal pain (may precede rash)
– Vomiting and diarrhoea, bloody stools, periumbilical pain
– Intussusception (about 5% patients)
– Rarely – Bowel perforation, major GI haemorrhage, pancreatitis and gallbladder hydrops.
Musculoskeletal
– Arthralgia and peri-articular swelling of joints, typically ankles and knees (synovial effusions typically absent) less commonly wrists, fingers and elbows.
– Decreased range of movement on examination, may be unable to weight bear
– No permanent deformity caused.
Renal
– Reported incidences – roughly 20-60% of cases
– Microscopic haematuria (most common), macroscopic haematuria, proteinuria, nephrotic syndrome, nephritis, acute renal failure, hypertension
– Of those who will develop renal involvement:
A) 75-80% of renal involvement occurs within 4 weeks
B) 97% of renal involvement occurs within 12 weeks
– Nephrotic presentation/Acute Renal Failure/Crescentic Glomerulonephritis on biopsy portend poorer prognosis for renal recovery than microscopic hematuria/mild proteinuria.
Other clinical manifestations of HSP include:
– Genital – scrotal swelling, painful ecchymotic induration of the scrotum, testicular pain, may mimic testicular torsion, testicular necrosis.
– CNS – headache, encephalopathy, intracranial haemorrhage, seizures, coma, Guillain‐Barre, cortical blindness (all rare)
– Pulmonary – haemorrhage (rare)
– Carditis
– Parotitis
Investigating suspected HSP:
There is no diagnostic test for HSP.
Investigations help to rule out other diagnoses.
In all patients:
– Weight and height
– Blood pressure
– Early morning Urinalysis weekly for 12 weeks(if proteinuria present, send for early morning urine protein creatinine ratio weekly)
Early morning (first voided) urinary protein/creatinine ratio(Normal range <20mg/mmol. significant proteinuria is >40, nephritic range is >200) or early morning urinaryalbumin/creatinine ratio(normal range <8mg/mmol, significant proteinuria > 200mg/mmol nephrotic range proteinuria >500mg/mmol)
– Baseline bloods– FBC, clottingand U&E
Also consider in some cases:
– Blood film, CRP, blood cultures if unsure of diagnosis or to rule out sepsis
– If evidence of renal involvement (suggested by hypertension, 2+ or greater proteinuria, or evidence of renal impairment on U&Es), check pANCA/cANCA, autoantibody screen, C3/C4 and discuss with a paediatric nephrologist.
There is no indication for renal USS unless specifically advised by nephrology team.
– Surgical referral if any suspicion of intussusception, bowel perforation, or testicular torsion, with investigations as guided by surgical team which may include erect CXR, AXR and USS abdomen.
Management:
– Supportive treatment – hydration, nutrition, electrolyte balance, monitor BP
– Analgesia – exercise caution in prescribing non-steroidal anti-inflammatories (contra-indicated in renal involvement, suggested by hypertension, 2+ or greater proteinuria, or evidence of renal impairment on U&Es)
– Information leaflet should be given to parents – with advice on seeking medical attention and training in urinalysis with open access to the ward. Parents should be advised that macroscopic haematuria or 3+ protein for 3 days should warrant urgent ward attendance. Prolonged 2+ protein can be seen in clinic
– If severe GI involvement consider the use of oral steroids (prednisolone 1mg/kg daily up to a maximum of 60mg daily) as a short course
– Discharge if well – pain controlled and no evidence of complications
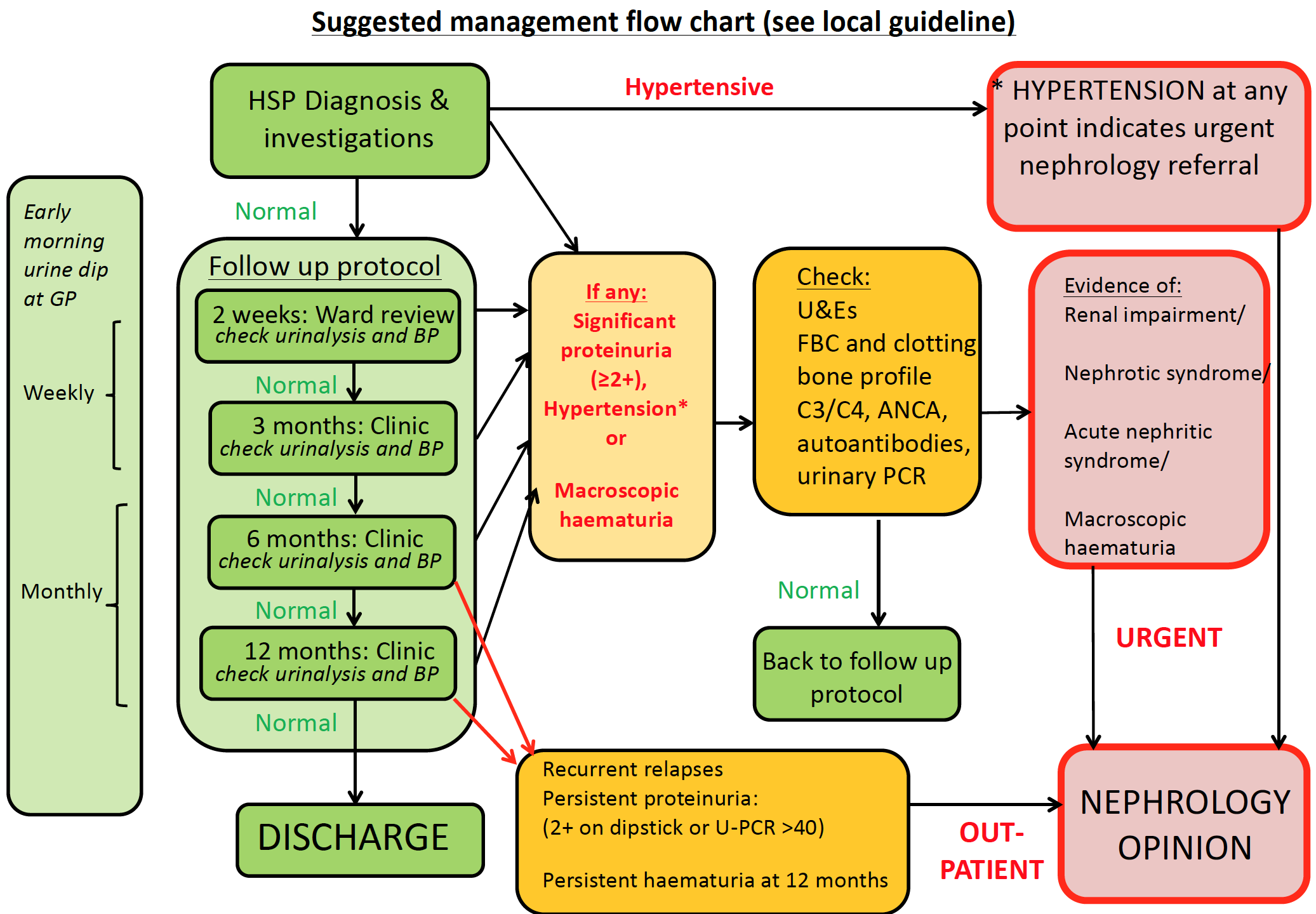
– Follow up – see below for thel management pathway for outpatient follow up
Further References:
1) Henoch Schonlein purpura. Tizard EJ, Hamilton-Ayres MJ. Arch Dis Child Educ Pract Ed 2008;93:1–8.
2) Risk of long term renal impairment and duration of follow up recommended for Henoch-Schönlein purpura with normal or minimal urinary findings: a systematic review. H Narchi. Arch Dis Child 2005 90: 916-920
