Paediatric Fluid calculations
Fluid requirements are different for enterally (orally/ NGT/ PEG) fed children to those who require IV fluids.
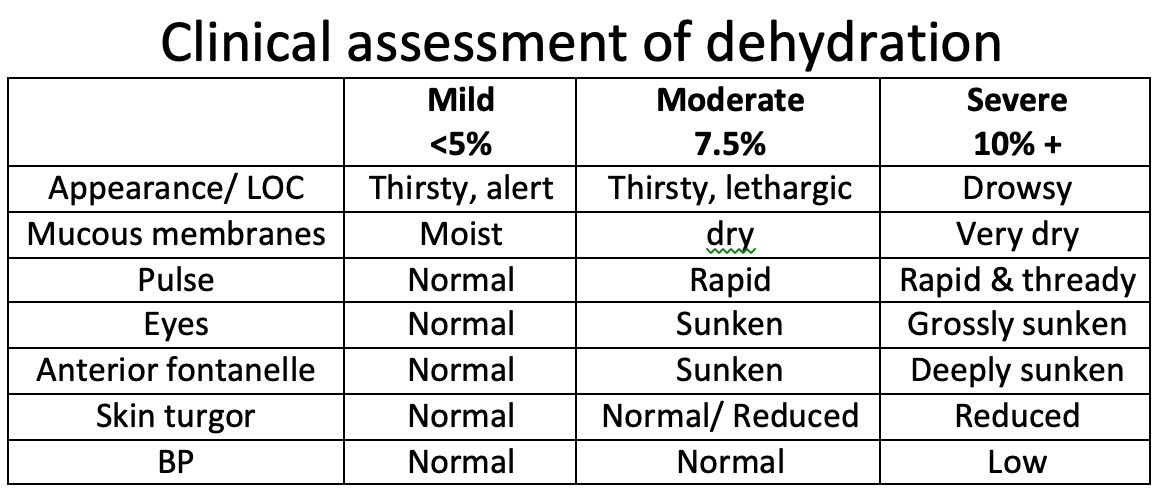
First review hydration status, any ongoing losses and any recent biochemistry results if available.
Remember that enteral fluids are always better if child able / allowed to feed/ drink.
Prescribing IV fluids in children:
You need to know weight of the child (exact or estimated) to calculate IV fluid requirements for the following situations:
– Maintenance fluid, if child kept Nil By Mouth or unable to tolerate orally/ enterally
– Deficit fluid, required to correct any dehydration
Maintenance fluids
Generally used fluids are 0.45% Saline with 5% Dextrose in younger children (infants to 10 years age) and 0.9% Saline in older children.
Potassium Chloride is sometimes added 10 – 20 mmol per 500ml bag if ongoing losses (eg. diarrhoea) or prolonged IVT, but monitor U&E
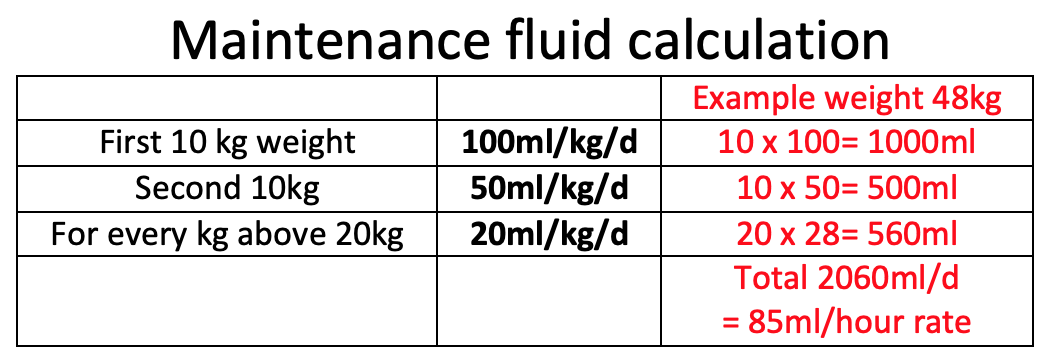
Formula to calculate maintenance fluids per day:
First 10kg of weight: Give 100mls/kg/24 hours
Second 10kg of weight: Add 50 mls/kg/24 hours
(ie for every kg above 10kg and up to 20kg)
For every kg above 20kg: Add 20 mls/kg/24 hours
(to a maximum of 80kg)
Deficit fluids
This amount is replaced in addition to maintenance fluids, generally spread over 24 to 48 hours.
Any fluid bolus gives is reduced from the total ‘deficit’ calculation.
Generally 0.9% saline is used/ the same fluid used for maintenance.
Formula to calculate fluid deficit:
Deficit (mls) = 10 x % dehydration x body weight (kg)
48kg child with 5% dehydration needs
Maintainence= 2060ml/d
Deficit = 10 x 48 x 5 = 2400ml/d
Bolus fluid for resuscitation:
A rapid fluid bolus of 0.9% Saline is used to expand circulating volume in shock, severe sepsis or significant blood loss.
Formula:
Fluid bolus (ml)= 20ml/kg over 20 to 30 minutes
Reassess after the bolus to ascertain if tachycardia is resolving, perfusion (CRT) is improving etc
Second fluid bolus may be required with another 20ml/kg Normal Saline if still in shock.
If patient has received 40ml/kg fluid bolus, this may cause pulmonary oedema- so call an anaesthetist, call seniors and inform PICU.
Note:
In certain situations, a smaller fluid bolus of 10ml/kg Normal Saline is used:
1) Newborn babies in sepsis or shock
2) DKA (risk of cerebral oedema)
3) In major trauma/ post-op/ Head injury
(as large fluid bolus may increase haemorrhage)
Replacement fluid
Any ongoing/ continuous losses (especially from GIT) is measures & replaced volume-for-volume every 6 to 8 hours.
Eg. if there is continuous loss of fluid from NGT on free drainage, stoma losses or drain losses- then measure amount lost in 6 hours & replace same volume (Normal Saline) over the next 6 hours in addition to other IV fluids that patient is receiving.
Formula:
Amount lost = amount to be replaced
Fluid restriction
In certain situations, patient is at risk of fluid overload, 3rd space loss, SIADH or vital organ complications- so the amount of daily ‘maintenance’ fluid is restricted.
Eg. after head injury, situations with raised intracranial pressure, severe bronchiolitis, etc
Formula:
To restrict at 75% amount= 0.75 x calculated daily maintenance fluids
NICE guideline. Intravenous fluid therapy in children and young people in hospital. (2015)
Feld LG et al. Clinical practice guideline: Maintenance intravenous fluids in children. Pediatrics 2018 Nov 26; 142:e20183083
