Acute Asthma
Acute severe asthma is a potentially life-threatening condition and requires urgent evaluation.
Consider differentials in a breathless child, like Foreign Body, Croup, Bronchiolitis, LRTI, Pneumothorax etc
Clinical Presentation
– Enquire about onset and duration of symptoms
– Trigger factor/s for current attack e.g. URTI, pollen, animal dander etc
– History of atopy in child & in family
– Usual medication/s and route of administration
– Compliance, use of spacer device and technique
– Frequency of attacks
– Previous hospital attendances / PICU admission
– Repeat courses of oral glucocorticoids
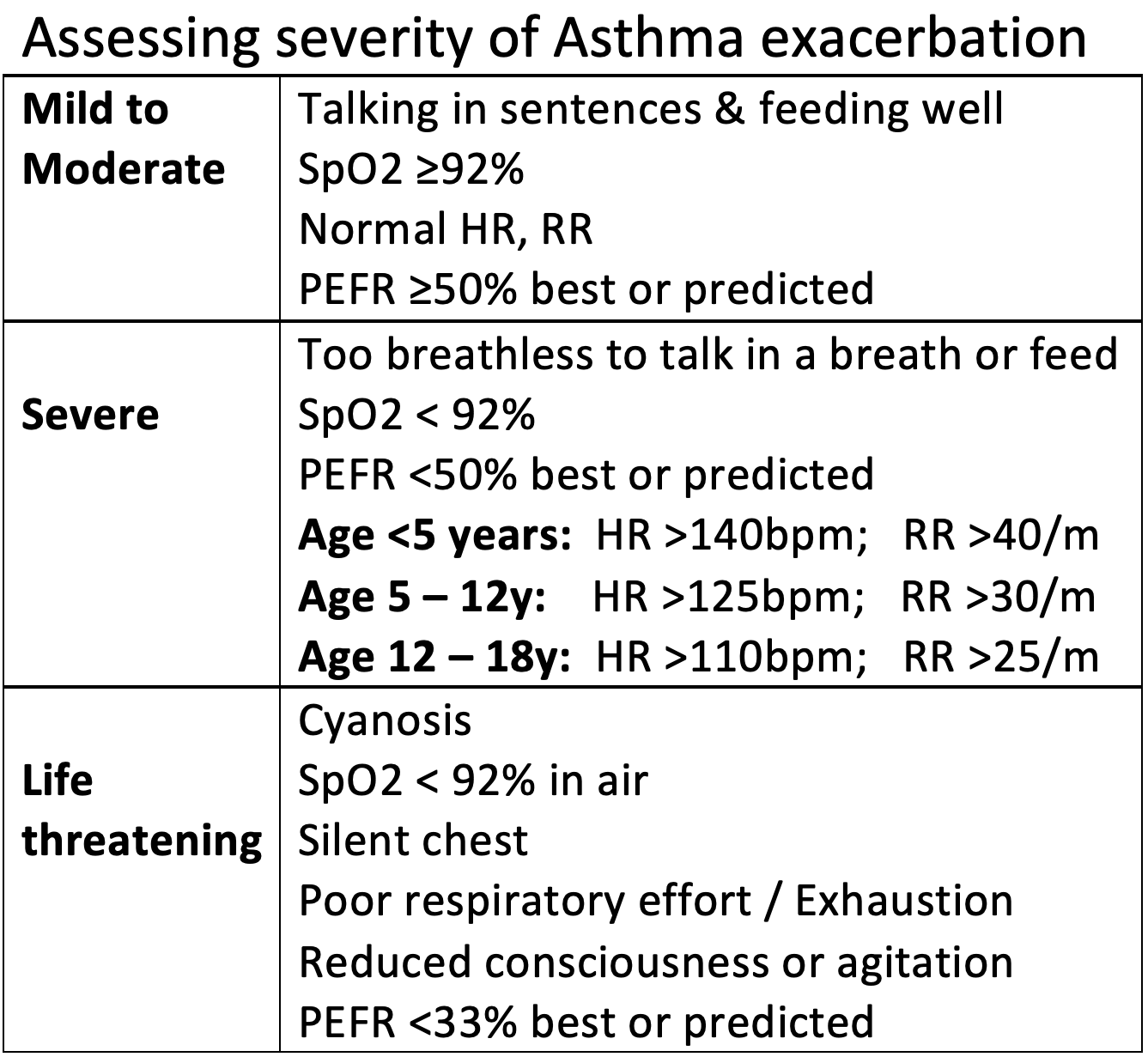
Rapid assessment to classify severity of attack, including:
– Temp, HR, RR, SaO2
– Audible wheeze
– Increased work of breathing?
– Level of consciousness
– Full respiratory examination
– Any signs of alternative diagnosis
(e.g. Foreign body, Pneumonia, Croup)
– PEFR in >5y age
– CXR only required if suspecting pneumothorax, consolidation or deterioration
Management
Mild to moderate episode:
Salbutamol by MDI+spacer then review after 15 minutes to decide on timing of next dose. Can be given every 30 – 60 minutes in moderate episode
Oral prednisolone even if discharging home for moderate episodes
Also continue any background inhaled Corticosteroids / Leukotriene antagonists
Discharge home if improving and will manage 3-4 hours between inhalers
Severe episode:
Inform senior doctors
Oxygen to keep SaO2 >92%
Salbutamol by MDI+spacer every 20 minutes for 1 hour;
review 15 min after 3rd dose.
Nebulised route if requiring Oxygen or not tolerating MDI+spacer
Ipratropium by MDI+spacer or Nebulised every 20 minutes for 1 hour only, then 4 to 6 hourly
Oral prednisolone (or Dexamethasone)
If improving, admit to ward and reduce frequency to 1-2 hourly with frequent reviews. Change back to MDI+spacer when not requiring O2 and clinically improving
If worsening, treat as life-threatening
Continue back-to-back Nebulised Salbutamol every 20 minutes for another hour
Give IV Magnesium sulphate & IV Hydrocortisone
Further 2ndline management as for Life threatening episode
Life threatening episode:
Initiate management as above for severe episode
Inform senior doctor, manage in HDU or resuscitation area if possible
Oxygen (high flow) to keep SaO2 >92%
Monitor SaO2, HR, RR (& ECG if escalating treatment)
Back-to-back nebulised Salbutamol & Ipratropium every 20 minutes
IV Hydrocortisone & IV Magnesium sulphate
IV Salbutamol Loading dose then continuous infusion; if required add
IV Aminophylline Loading (often adequate improvement) or follow with continuous infusion
– Consider CXR to exclude Pneumothorax/ alternative diagnosis
– Check CapGas/ ABG to monitor pH & pCO2
– Check U&E if prolonged Salbutamol therapy to check Potassium
Seek PICU & Anaesthetic input for ongoing management, as ventilation can be difficult in severe Asthma
Inform PICU for transfer if:
– Life threatening features with no immediate response to treatment
– Consider if previous admissions have always required PICU treatment
– No improvement with IV salbutamol or loading dose of aminophylline
– Hypoxia persisting or worsening
– Exhaustion / shallow respirations, respiratory arrest or confusion or coma
At discharge, ensure:
– Inhaler and Spacer technique checked
– Discharge letter to include severity of episode, triggers, previous control
– Allergen avoidance advice given, including smoking cessation
– Home Asthma management plan to be provided, including when to seek help
– Follow up arranged – as appropriate
*All doses as per local policy
James DR, Lyttle MD. British guideline on the management of asthma: SIGN Clinical Guideline 141, 2014 Archives of Disease in Childhood – Education and Practice 2016;101:319-322.
White J, Paton JY, Niven R on behalf of the British Thoracic Society, et al. Guidelines for the diagnosis and management of asthma: a look at the key differences between BTS/SIGN and NICE Thorax 2018;73:293-297.
